
Common corneal disorders can be broadly categorized into ocular surface disorders, ectatic disorders, infectious disorders, and corneal degenerative and dystrophic conditions. These conditions can significantly affect corneal health, leading to vision impairment and discomfort. If you are experiencing any corneal issues, consulting a cornea specialist in Hyderabad is essential for accurate diagnosis and advanced treatment. At a leading cornea clinic in Hyderabad, Telangana, patients receive specialized care for various corneal conditions, ensuring optimal eye health. Seeking treatment from the best cornea specialist in Hyderabad can help prevent complications and restore clear vision with advanced medical and surgical interventions. For comprehensive eye care, visiting the best eye hospital in Hyderabad ensures access to cutting-edge technology and experienced professionals. Whether you need expert consultation from an eye specialist in Hyderabad or a highly skilled eye specialist doctor in Hyderabad, choosing the right medical facility plays a crucial role in effective treatment and long-term eye wellness. If you need specialized corneal care, consult a trusted cornea specialist in Hyderabad today and take the first step toward clearer, healthier vision.
The cornea is a vital part of the eye that plays a crucial role in vision. Daily care and protection of the cornea are essential to maintain good eye health. Here are some tips to ensure the well-being of your cornea:






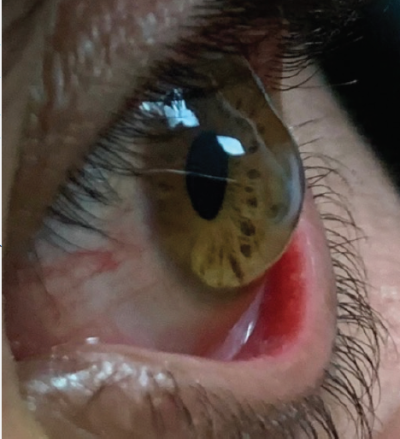
Common corneal disorders can be broadly categorized into ocular surface disorders, ectatic disorders, infectious disorders, and corneal degenerative and dystrophic conditions. Each category encompasses a variety of conditions that can affect the cornea’s health and function, impacting vision and overall eye wellness.

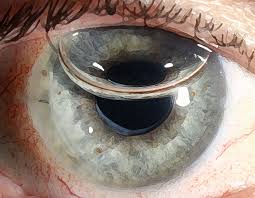
A progressive thinning and bulging of the cornea, resulting in distorted vision. It is often treated with specialized contact lenses, corneal cross-linking, or corneal transplant.
Pellucid Marginal Degeneration a thinning of the cornea along its lower edge, causing irregular astigmatism and visual impairment.

Posterior Keratoconus a rare condition where the back surface of the cornea becomes steepened, which may lead to visual distortion and require monitoring.
Before the surgery, patients undergo a thorough evaluation to assess their overall health and suitability for the procedure. Pre-operative tests may include blood tests, imaging, and a complete eye examination. Patients may need to stop certain medications prior to the surgery.
Recovery from corneal transplants can vary depending on the type of procedure and individual patient factors. Patients may experience discomfort and vision fluctuations in the initial days or weeks after surgery. Post-surgery care includes using prescribed eye drops to prevent infection and inflammation, as well as attending follow-up appointments for monitoring progress.
While corneal transplants are generally safe, potential risks and complications include
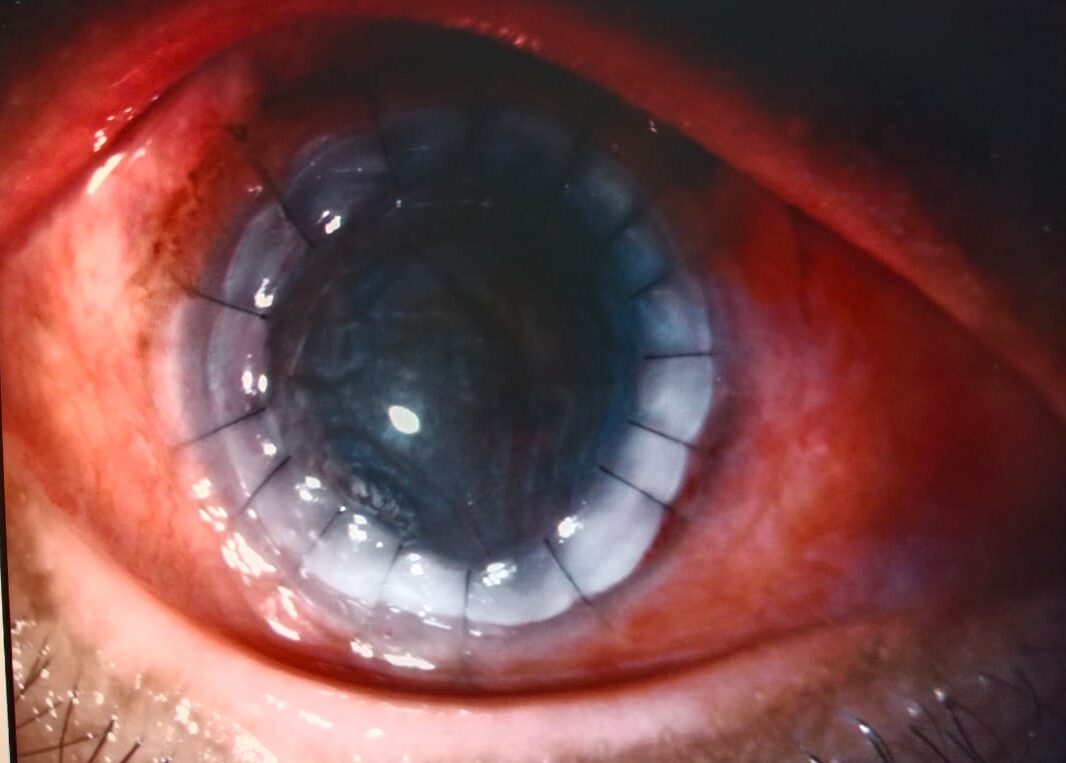

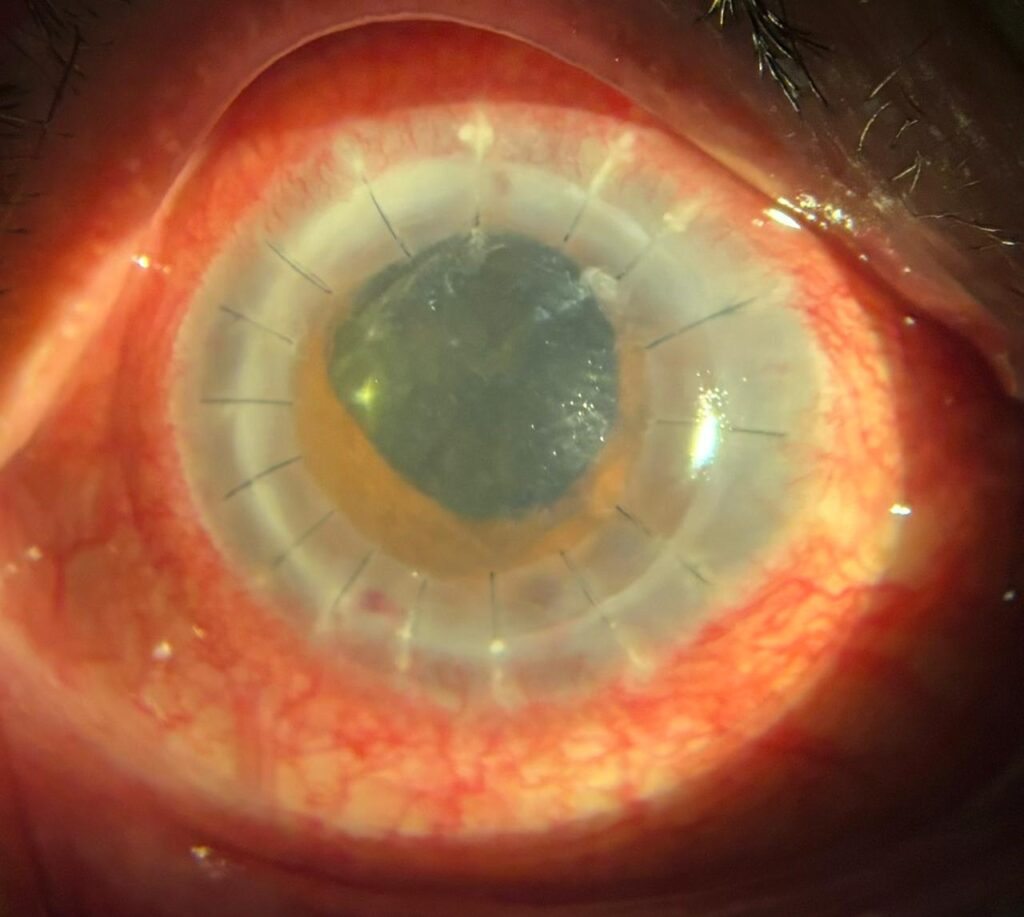
These different types of corneal transplants offer various options to address specific corneal issues. The choice of procedure depends on the patient’s condition, the surgeon’s expertise, and the expected outcomes.
Shanthi Nethralaya Eye Hospital is a premier choice for corneal transplant surgeries due to the expertise and experience of Dr. Shanthiniketh, who performs these procedures at the hospital. Here are several reasons why patients may choose Shanthi Nethralaya for corneal transplant surgeries

Training at LVPEI: Dr. Shanthiniketh received specialized training at L.V. Prasad Eye Institute (LVPEI), a renowned eye care center known for its excellence in ophthalmology. This training has equipped him with advanced skills and knowledge in corneal surgeries. Extensive Experience: Dr. Shanthiniketh has performed over 1,000 eye transplants throughout his career, demonstrating his proficiency in a wide range of corneal procedures, including advanced lamellar techniques.Continuous Learning: Dr. Shanthiniketh stays updated on the latest advancements in corneal transplant surgeries, ensuring patients receive the most effective and modern care.

Development of Cornea Department: Dr. Shanthiniketh has been instrumental in developing the cornea department at Akira Eye Hospital in Rajahmundry, enhancing the quality of eye care in the region. Chief Cornea Consultant: Dr. Shanthiniketh serves as the chief cornea consultant at Neoretina Eye Hospital, part of the Centre for Sight group of hospitals, contributing his expertise to another esteemed institution.

Personalized Care: Patients receive individualized treatment plans tailored to their specific needs, from preoperative assessments to postoperative follow-up care. Advanced Surgical Techniques: Shanthi Nethralaya employs cutting-edge techniques such as Descemet's membrane endothelial keratoplasty (DMEK) and Descemet's stripping endothelial keratoplasty (DSEK), ensuring precise and successful procedures. Comprehensive Postoperative Support: The hospital offers thorough postoperative care, including regular follow-up visits and personalized guidance for optimal recovery.

Patient Education: Dr. Shanthiniketh prioritizes educating patients about their condition, the surgical process, and postoperative care, empowering them to make informed decisions about their eye health. Comfort and Convenience: Shanthi Nethralaya's facilities are designed to provide a welcoming and supportive environment for patients.
In summary, Shanthi Nethralaya Eye Hospital offers top-notch corneal transplant surgeries with the exceptional expertise of Dr. Shanthiniketh, backed by his training at LVPEI and commitment to personalized, high-quality care. The hospital’s focus on patient education and comprehensive support ensures optimal outcomes and patient satisfaction.

WhatsApp us