Keratoconus changes the shape and structure of your cornea, affecting how light enters your eye. This can lead to blurry or distorted vision and other symptoms such as increased sensitivity to light. Let’s explore the causes of this condition and how it can be treated. Our hospital offers advanced keratoconus treatment options tailored to individual patient needs.





If you’re noticing any of these symptoms, it’s essential to have your keratoconus eye thoroughly examined by a specialist.

Measures how clearly you can see.

Measures how light is reflected by your retina.

Assesses the cornea and other structures.

Measures corneal thickness.

Creates a detailed map of the cornea’s shape and thickness, essential for diagnosing and monitoring keratoconus.
At Shanthi Nethralaya, we provide comprehensive treatment for keratoconus, from early management to advanced surgical procedures.

Helpful in early stages.

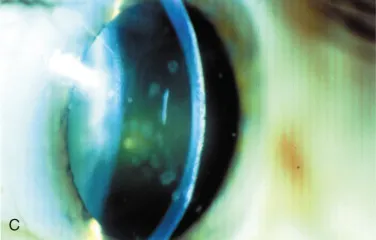
Specialty lenses like RGP and scleral lenses provide better visual correction.
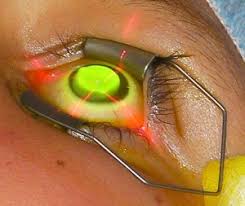
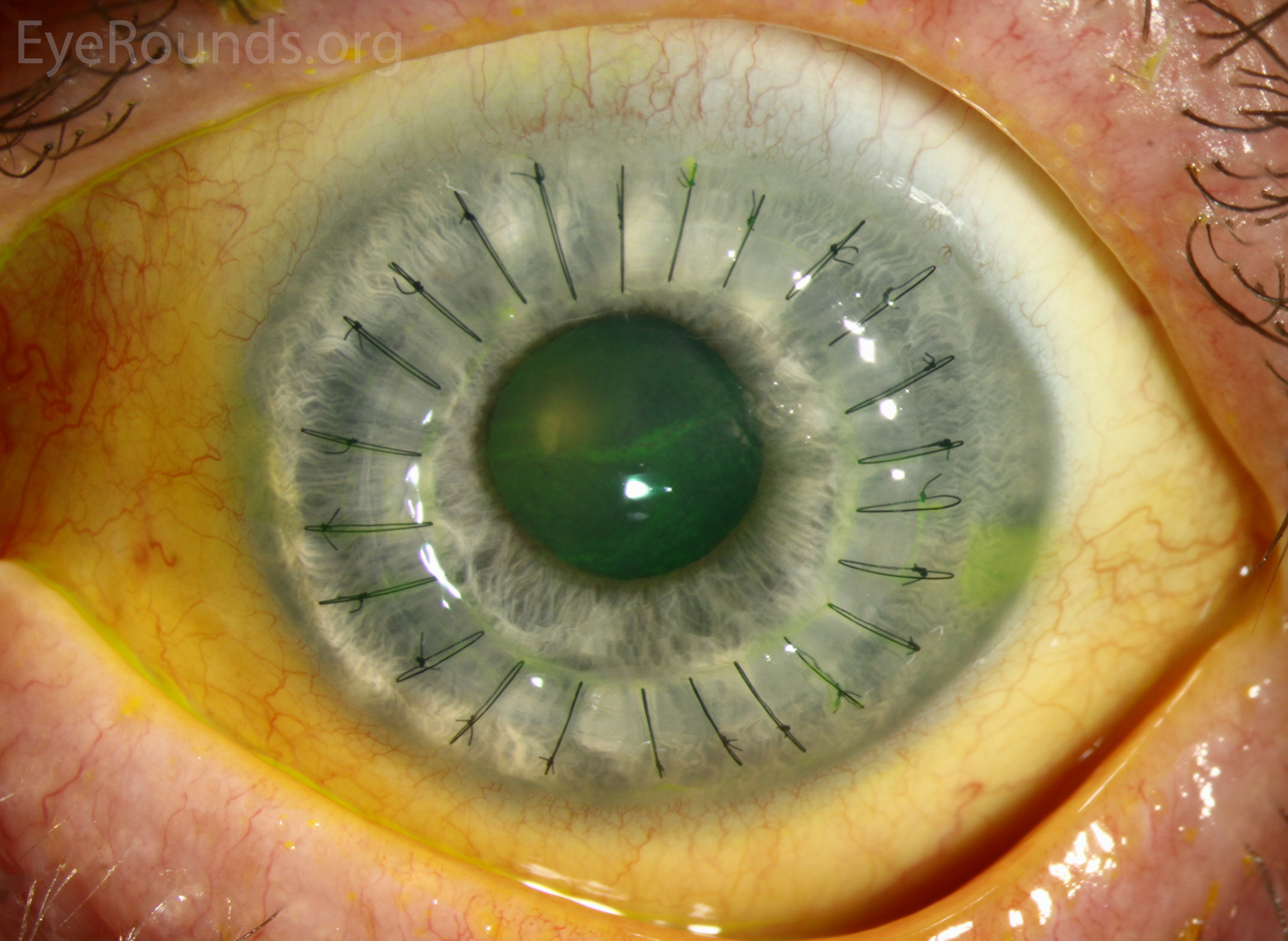
A minimally invasive keratoconus surgery using riboflavin drops and UV light to strengthen the cornea and stop progression.
A combination of CXL and PTK laser treatment for improved visual outcomes.
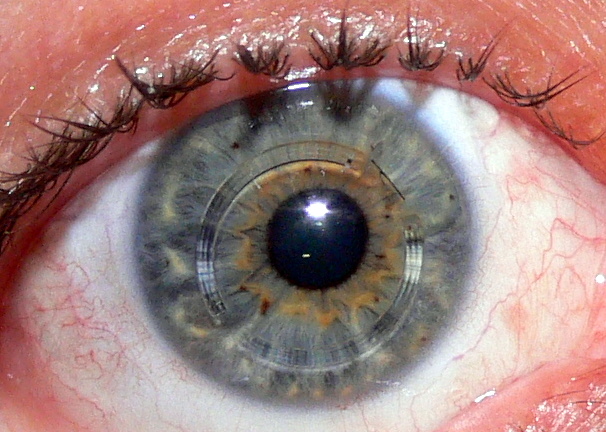
Tiny rings placed in the cornea to reshape it and improve vision.
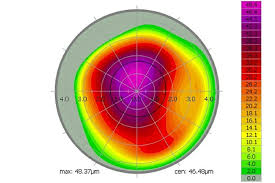
A laser-based reshaping procedure using corneal maps.
A partial-thickness corneal transplant that preserves the inner corneal layer.
Our experienced surgeons specialize in various keratoconus surgery techniques, ensuring optimal results for each patient.



From diagnostics to surgery, we use the latest tools to deliver precision care.
Continuous monitoring and follow-ups after treatment ensure recovery and success.

Our keratoconus specialists are known for their expertise in handling complex cases with care and confidence.
Whether it’s connecting you with keratoconus support groups or providing additional information about your condition, we’re here for you every step of the way.
Patients who have received treatment from me at Shanthi Nethralaya have experienced significant improvements in their vision and quality of life. The hospital’s reputation speaks for itself!
Our center is trusted by many for providing effective and personalized keratoconus treatment, with a focus on improving vision and quality of life.
Surgery costs can vary depending on the procedure and the healthcare provider.Let’s talk about the different options and costs that could work for you.
This can slowC3R, or corneal cross-linking, helps strengthen the cornea with special eye drops and UV light.down or stop the progression of keratoconus.

WhatsApp us