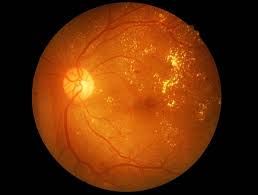
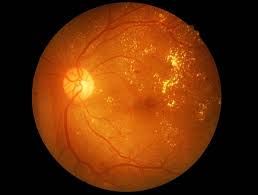
Non-Proliferative Diabetic Retinopathy (NPDR)
In the early stages, the damaged blood vessels may leak fluid or blood into the retina.
Diabetic retinopathy occurs when high blood sugar levels cause damage to the tiny blood vessels in the retina, the part of your eye that senses light and sends signals to the brain. Over time, this damage can lead to vision problems, including blurriness, floaters, or even vision loss. As a leading retina eye hospital in Hyderabad, Shanthi Nethralaya offers advanced care for diabetic retinopathy and other retinal disorders. With a team of highly experienced professionals, we ensure timely diagnosis and expert treatment for every patient.
Your doctor will ask about your symptoms, medical history, and any known allergies.
If you have diabetes, regular eye exams are crucial, even if you aren’t experiencing any vision problems. Early detection of diabetic retinopathy can prevent vision loss and help manage your eye health effectively. Patients looking for a trusted retina specialist in Hyderabad can count on Shanthi Nethralaya for reliable and expert care.

It’s recommended that all individuals with diabetes have a comprehensive dilated eye exam at least once a year. At Shanthi Nethralaya, our retina specialist doctors in Hyderabad conduct thorough screenings using the latest diagnostic technology.

Blurred vision, floaters, dark spots, or sudden vision changes should prompt an immediate visit to your eye doctor. Our retina unit, staffed by the best vitreo retinal surgeon in Hyderabad, is well-equipped to address such conditions swiftly and effectively.

If you are planning to become pregnant, an eye exam is essential as pregnancy can increase the risk of diabetic retinopathy progression. Shanthi Nethralaya is considered one of the best eye hospital in hyderabad for retina specialist services, especially for patients who require special attention during pregnancy.
A dilated eye exam allows the eye doctor to see the back of your eye (the retina) more clearly. During this exam, eye drops are used to widen (dilate) your pupils, allowing for a detailed examination of your retina and blood vessels. These exams are a critical part of care offered at our retina eye hospital in Hyderabad, where early detection is a priority.
In addition to diabetic retinopathy, diabetes can increase your risk of developing other eye conditions, including:
While it may not be possible to completely prevent diabetic eye conditions, you can reduce your risk by managing your diabetes effectively:
Our expert team, including some of the best retina specialist doctors in Hyderabad, is here to guide you in protecting your vision for the long term.
Protecting your vision is a vital part of managing your diabetes. Regular eye exams are key to detecting diabetic retinopathy and other eye conditions early, allowing for effective treatment and prevention of vision loss. Contact Shanthi Nethralaya – a trusted retina eye hospital in Hyderabad – today to schedule your diabetic eye exam and take the next step in safeguarding your vision.
Diabetic retinopathy is an eye condition that affects people with diabetes. It occurs when high blood sugar levels damage the blood vessels in the retina, leading to vision problems. If left untreated, it can result in vision loss or blindness.
Anyone with diabetes—whether Type 1, Type 2, or gestational diabetes—is at risk of developing diabetic retinopathy. The risk increases with the duration of diabetes and poor control of blood sugar levels. Other factors such as high blood pressure, high cholesterol, and smoking can also increase the risk.
Diabetic retinopathy is often detected during a comprehensive dilated eye exam. Your eye doctor will use special drops to dilate (widen) your pupils, allowing them to see the retina more clearly. Retinal imaging may also be used to capture detailed images of the retina and blood vessels, helping to detect any early signs of retinopathy.
Diabetic retinopathy progresses through two main stages:
In addition to diabetic retinopathy, people with diabetes are at higher risk for other eye conditions, including:
It is recommended that people with diabetes have a comprehensive dilated eye exam at least once a year. More frequent exams may be necessary if you have been diagnosed with diabetic retinopathy or if your blood sugar levels are not well controlled. Early detection is key to preventing vision loss.
In the early stages, diabetic retinopathy often has no noticeable symptoms. As the condition progresses, you may experience:
The treatment for diabetic retinopathy depends on the stage and severity of the condition. Options include:
Diabetic retinopathy cannot be completely cured, but its progression can be slowed or stopped with timely treatment and proper management of diabetes. Early detection through regular eye exams is crucial for preventing severe vision loss.
The prognosis for diabetic retinopathy varies depending on how early the condition is detected and how well it is managed. With early intervention and good control of blood sugar, blood pressure, and cholesterol, many people with diabetic retinopathy can preserve their vision. However, if left untreated, it can lead to severe vision impairment or blindness.
While diabetic retinopathy may not always be preventable, you can reduce your risk by:
If you’ve been diagnosed with diabetic retinopathy, it’s essential to follow your eye doctor’s recommendations closely. This may include regular monitoring, treatment such as laser therapy or injections, and strict management of your diabetes. Early intervention can significantly improve your prognosis and help prevent vision loss.
This FAQ section is designed to inform patients about diabetic retinopathy, encourage regular screenings, and explain available treatments and prognosis. Let me know if you’d like to add or adjust any of the content!
Unfortunately, diabetic retinopathy is not reversible. However, its progression can be slowed or halted with proper management and treatment. Early detection through regular eye exams is crucial to prevent irreversible damage.
High blood sugar levels can damage the small blood vessels in the retina, leading to leaks or blockages. Over time, this can cause blood and fluid to seep into the retinal tissue, damaging the retina and impairing vision. High blood sugar can also trigger the growth of new, abnormal blood vessels that are prone to bleeding and scarring.
Yes, diabetic retinopathy can develop silently, without noticeable symptoms, especially in its early stages. That’s why regular eye exams are vital for people with diabetes, even if they feel their vision is normal. By the time symptoms occur, the condition may already be advanced.
If left untreated, diabetic retinopathy can progress to more severe stages, potentially leading to serious complications such as:
Diabetic retinopathy can impact daily activities such as reading, driving, and recognizing faces. Vision changes may make it difficult to perform tasks that require clear vision. Early intervention can help maintain your ability to carry out daily activities, but advanced stages of retinopathy may require lifestyle adjustments.
No, diabetic retinopathy requires a comprehensive dilated eye exam to be detected. A standard vision screening, which typically tests your visual acuity (clarity of vision), may not detect changes in the retina. It’s essential for people with diabetes to undergo dilated eye exams regularly.
While diabetic retinopathy can occur at any age in people with diabetes, it is more likely to develop in those who have had diabetes for many years. People over the age of 40 with Type 2 diabetes or those who have had Type 1 diabetes for over 20 years are at higher risk for developing retinopathy.
Yes, pregnancy can worsen diabetic retinopathy, especially in women with pre-existing diabetes. It’s important for women with diabetes who are planning to become pregnant to have a comprehensive eye exam before pregnancy and follow up with regular exams throughout their pregnancy to monitor for any changes.
Controlling blood sugar helps prevent damage to the blood vessels in the retina. Consistently high blood sugar levels can weaken blood vessel walls, leading to leakage, swelling, and abnormal blood vessel growth. Keeping blood sugar levels within your target range reduces the risk of developing diabetic retinopathy or slowing its progression if it has already begun.
Lifestyle changes that can help prevent or manage diabetic retinopathy include:
Laser treatment and injections for diabetic retinopathy can slow the progression of the disease and prevent further vision loss, but they do not cure the condition. These treatments are most effective when the condition is detected early. Continuous management of your diabetes and regular eye exams are essential even after treatment.
Yes, stress can indirectly affect diabetic retinopathy by impacting blood sugar levels. When you’re stressed, your body releases hormones like cortisol, which can increase blood sugar levels. Poorly managed stress can lead to fluctuations in blood sugar, which may worsen diabetic retinopathy. Managing stress through relaxation techniques, exercise, and proper medical care can help control blood sugar levels and reduce the risk of complications.
Diabetic retinopathy usually affects both eyes, although the severity can differ between the two. It’s important to monitor the condition in both eyes through regular check-ups. Treatment plans are often customised based on the condition’s progression in each eye.
There are no home remedies or supplements proven to cure or prevent diabetic retinopathy. The best way to manage the condition is through medical treatment, blood sugar control, and regular eye exams. Some studies suggest that a healthy diet rich in antioxidants may support eye health, but these should complement, not replace professional medical care.

WhatsApp us